“A lot.”
That’s what radiologists don’t know about MIPS, aka the Merit-based Incentive Payment System.
So says radiology economics expert Lauren Golding, MD, who is vice chair of the American College of Radiology’s MACRA Committee.
She’s speaking from unassailable observation. In 2017, 60 percent of physicians reported being “not at all familiar” or “slightly familiar” with MACRA—the Medicare Access and CHIP Reauthorization Act, the legislation that created MIPS—and only 8 percent indicated being “very familiar,” according to a study published the July 2018 edition of Health Affairs. The survey was conducted during the first year of the program, but anecdotal evidence strongly suggests the lack of understanding persists.
The primary problem is that MIPS is far too complicated for its own good, says Golding, who practices with Triad Radiology Associates in Winston-Salem, N.C. “Only a handful” of physicians truly grasp MIPS, she says. “It’s really hard to get a handle on the specifics, the program’s little nuances. The average clinician can’t really understand what they’re being measured on and how they’re going to sort it out.”
This complexity was one reason MedPAC, the Medicare Payment Advisory Commission, has recommended that MIPS be re-thought. (See “MedPAC Wants MIPS to Go Away. Should the Group Get Its Way?” in the December issue of RBJ.)
Come what may, clinicians have a little more time to sort through the morass. Originally, MIPS was to be up and humming as of this year, but Congress delayed full implementation until 2022.
The experts have one message for the procrastinators: Put the systems and processes in place this year—or risk hefty penalties down the road.
The Basics: A Refresher
MACRA created the Quality Payment Program (QPP) to replace the Sustainable Growth Rate reimbursement formula. QPP has two primary tracks. MIPS provides performance-based adjustments to Medicare payments. Advanced APMs—Advanced Alternative Payment Models—require networks to assume financial risk for their patients. There’s much to recommend APMs, especially as the QPP matures, but for now nearly all radiologists are on the MIPS track.
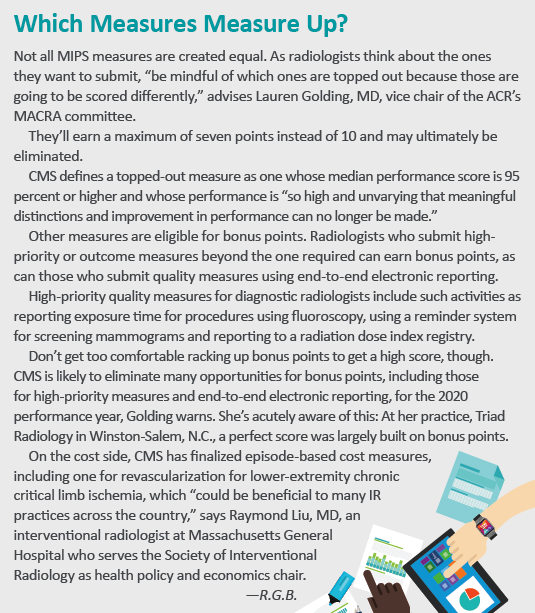
MIPS has four differently weighted performance categories: Quality (45 percent), Cost (15 percent), Promoting Interoperability (25 percent) and Practice Improvement Activities (15 percent). Bonus points are available, but the cap is set at 100 points (which would reflect a perfect score of 100 percent). Additionally, practices that score at least 75 (up from 70 last year) are eligible to share in the $500 million Exceptional Performance Bonus, a separate pool of money.
Almost all radiologists are required to participate. The only exceptions:
- Those in their first year of Medicare Part B participation.
- Those with a low volume of Medicare Part B patients in a 12-month period: (a) billing $90,000 or less under Part B; (b) providing care for 200 or fewer Part B beneficiaries; or (c) delivering 200 or fewer covered services to Part B beneficiaries.
- Those participating in an Advanced APM.
Notably missing from this list is “does not see patients,” points out Ezequiel Silva III, MD, who practices with South Texas Radiology and serves as chair of the ACR’s commission on economics. Silva has encountered the perception that, if radiologists aren’t deemed “patient-facing,” they are exempt from reporting. They are not. They merely have a “somewhat lighter burden.”
Losers Pay
MIPS is budget-neutral, so the pool for the bonuses comes from the penalties assessed. Put simply, the losers pay the winners. Many radiologists may not understand the full implications of budget neutrality, Silva warns. “We’re actually being scored and compared relative not just to other radiologists,” he says, “but to other specialists across all of medicine.”
That lack of understanding is, well, understandable: It was hard not to earn a bonus in the first year, with 93 percent of 1.06 million eligible clinicians receiving a payment, according to CMS. Two percent received a neutral adjustment, and 5 percent received a penalty.
“The positive adjustment is pretty measly in terms of dollars,” Golding says. In year one, for instance, both Golding’s and Silva’s practices had perfect scores. But the bonus—received this year—amounted to only 1.88 percent because so few clinicians came in below the threshold.
CMS increased the MIPS performance threshold for neutral adjustments to 15 points in 2018 and 30 points in 2019. This may seem substantial, but it’s not, considering that MIPS was supposed to be fully implemented by now. That means winners will still outnumber losers.
For 2019, the penalty/bonus is 7 percent, but again, since winners will outnumber losers, it’s unlikely anyone will earn a 7 percent bonus even with a perfect score.
Once MIPS is fully implemented in 2022, clinicians could earn bonuses as high as 37 percent or face penalties of up to 9 percent. The threshold will be the mean or median, yielding winners and losers in about equal headcounts.
The financial bonus may be meager now, but it won’t be forever. The extended ramp-up period gives practices the opportunity to ensure robust bonuses down the road. But the easy early years may make some overconfident: Radiologists may think they are on track when they are actually facing a penalty down the road.
“Practice now and get good at it,” Golding counsels. Those who have been working on MIPS from the beginning will have an advantage over those forced to catch up.
And that advantage relates to much more than money.
 Demonstrating Value
Demonstrating Value
MIPS is about much more than its incentive program. “It’s more than dollars. It’s also your public reputation at stake,” says Luke Ginocchio, MD, a radiology resident at NYU Langone Health. For example, CMS publishes an array of clinician-identifiable performance measures through its Physician Compare website. Those measures include the MIPS score and performance category scores. All are publicly available.
Most of the things involved in complying with MIPS “will be necessary for your success in the future,” Golding says. She urges radiologists not to ignore the business case. This is preparation, she suggests, for success in a value-based world.
For example, she points out, some radiologists in academic or multispecialty groups don’t think MIPS matters to them, assuming the primary care physicians in the practice will handle it.
They could leave it to the PCPs, but that would be shortsighted, Golding warns. “A radiologist can submit measures and do quality measures just like anyone else,” she says. “Each group will submit the six measures it performs the best. Maybe some of those are radiology measures.”
Submitting and excelling on MIPS radiology measures provides an excellent way to demonstrate value to the group, Golding says, adding this will become increasingly important in the move to value-based care, accountable care organizations and other risk-sharing models. “Radiology really does need some concrete way,” she says, “to show how we are contributing.”
MIPS results to date indicate those who report as groups score better than those who do so as individuals. Silva expects most radiologists to take the former route.
 Registering Progress
Registering Progress
The consensus, not just among radiology leaders but across specialties, is this: Submit your data through a Qualified Clinical Data Registry (QCDR). “I think that the radiologists who really are committing themselves to be successful in this program have to have a strong presence in the quality category which means a strong presence on the registry,” Silva says.
The cost category, based on claims data, requires no reporting. But the other three—Quality, promoting Interoperability and Improvement Activities—and claims data will no longer be accepted for practices with more than 15 eligible clinicians. This means that, for most practices, registries are the way to go.
The ACR National Radiology Data Registry (NRDR) is a CMS-approved QCDR. It includes patients across all payers and allows practices to also submit custom quality measures, not just MIPS measures. These QCDR measures are reviewed and approved by CMS annually and allow clinicians greater flexibility to select measures which may be more applicable to their practices.
Interventional radiologists have a comparable registry: the National Quality Interventional Radiology Registry from ACR and SIR.
These registries allow radiologists to collect data, monitor performance relative to other practices and, of course, report to CMS. Using them also helps improve healthcare delivery in general, Silva says. “It gives to the greater good because now you have larger pools of data to help inform policy decision-making and things of that sort—population health, if you will.”
Although many reporting duties can be delegated, they cannot be left solely to the billing and coding team.
“I don’t really view it as either/or but complementary,” says Luke Ginocchio, MD, of NYU Langone Health, lead author of “A Wake-up Call to Avoid Penalties Under MACRA” (JACR, February 2018).
“Work very closely with your billers and your coders,” Ginocchio says. “They are the experts in what they do. The radiologist brings the clinical perspective. We know which measures make sense for our practices. We know which ones we can really optimize and do well in.”
To make this effective, each practice needs a QPP champion—a registry champion who understands the registry enough to make meaningful quality improvements, say Golding and Silva. They need to look at the data from a clinical perspective and communicate to their partners. That doesn’t preclude delegating the bulk of the work, but it does mean staying deeply involved in the process.
Haven’t begun using a registry yet? That’s not a problem. It’s not too late to use one for 2019, Silva says. But you should start now.
Approach it from a quality perspective vs. a “check the box” perspective. It comes back to a central question, says Golding. “Are you just playing the game to get the reward or are you really making a difference that is going to help your practice be sustainable in a value-based system?”
A Reprieve for the Unprepared
In 2019, the composite performance score was to have been either the mean or a median—again, half winners, half losers. Instead, Congress, under the Feb. 2018 Bipartisan Budget Act, modified MACRA to allow CMS to further delay MIPS imple-mentation until 2022.
CMS increased the MIPS performance threshold for neutral adjustments from 15 to 30 points in 2019. This threshold defines the total points required to avoid a negative payment adjustment. That means if you earn more than 30 points in 2019, you avoid a penalty and may earn a bonus for 2021.
“There was supposed to be a lot more at stake,” Golding says, underscoring that 2019 was supposed to be the year where the program was fully implemented. “That means there would be a whole lot of losers in the program and a lot more money available to be distributed among the winners.”
What changed? Congress recognized that most physicians weren’t ready for full implementation. “So they’re keeping the program in the ramp-up phase,” Golding says. “The stakes are getting higher, but they’re not as high as they would have been without intervention from Congress.”
MIPS could change again. In fact, it could even be abolished, if Congress listens to MedPAC and does indeed scrap the whole thing, notes Ginocchio. “MedPAC is strongly advocating that Congress do that,” he says, “but there’s no indication Congress is taking it seriously.”
Then too, these are volatile times in Washington. Today’s lack of indication on anything may be tomorrow’s change of mind on everything. Don’t stop watching the news.
